We aim to provide and promote an efficient and effective, high quality breast screening service, to all eligible women within a caring environment.
The North Lancashire and South Cumbria Breast Screening Service is part of the National Breast Screening Programme and provides a free breast screening service for eligible well women in North Lancashire and South Cumbria.
Breast screening aims to find breast cancer at an early stage, often before there are any symptoms. To do this, an x-ray (mammogram) is taken of each breast. Early detection may often mean simpler and more successful treatment.
Public Health England (PHE) created this information on behalf of the NHS. In this information, the word ‘we’ refers to the NHS service that provides screening.
Source NHS breast screening: helping you decide - GOV.UK (www.gov.uk)
It is your choice whether to have breast screening or not. This information aims to help you decide.
Why the NHS offers breast screening
The NHS offers screening to save lives from breast cancer. Screening does this by finding breast cancers at an early stage when they are too small to see or feel. Screening does not prevent you from getting breast cancer.
Breast screening does have some risks. Some women who have screening will be diagnosed and treated for breast cancer that would never otherwise have been found or caused them harm.
Why you have been invited for breast screening
All women aged 50 up to their 71st birthday are invited for breast screening every 3 years. We send out first invitations to screening some time between your 50th and 53rd birthdays.
If you are aged 71 or over, you are still at risk of breast cancer. Although you will no longer receive screening invitations after your 71st birthday, you can still have breast screening every 3 years. You will need to ask your local breast screening unit for an appointment. Find details of your local breast screening unit on the NHS.UK website.
Some local breast screening services may send you SMS (text) appointment reminders for breast screening.
Breast cancer
Breast cancer starts when cells in the breast begin to grow in an uncontrolled way and build up to form a lump (also known as a tumour). As the cancer grows, cells can spread to other parts of the body and this can be life-threatening.
Breast cancer is the most common type of cancer in the UK. About 12,000 women in the UK die of breast cancer every year. Survival from the disease has been improving over time, and now about 3 out of 4 women diagnosed with breast cancer are alive 10 years later.
Your risk of getting breast cancer goes up as you get older. About 4 out of 5 breast cancers are found in women over 50 years old. Most women with breast cancer do not have a family history of the disease.
Breast screening
Breast screening uses an X-ray test called a mammogram to check the breast for signs of cancer. It can spot cancers that are too small to see or feel.
Choosing to have breast screening
When you arrive at the breast screening unit, the staff will check your details and ask you about any breast problems you have had. If you have any questions, please ask.
Mammograms are carried out by women called mammographers. The mammographer will first explain what will happen. She will then place your breast onto the mammogram machine and lower a plastic plate onto it to flatten it. This helps to keep your breast still and get clear X-rays.
The mammographer will usually take 2 X-rays of each breast, one from above and one from the side. She will go behind a screen while the X-rays are taken. You have to keep still for several seconds each time.
The whole appointment takes less than 30 minutes and the mammogram only takes a few minutes.
You may be asked if you want to take part in a clinical trial
These are medical research studies. Any trial you are offered will gather information about the best types of breast cancer tests or treatments so we can help women more effectively in the future. You can choose whether to take part or not.
Preparing for your mammogram
To have a mammogram, you need to undress to the waist. So it may be easier to wear a skirt or trousers instead of a dress.
Please do not use a spray deodorant or talcum powder as this may show up on your mammogram. You can use roll-on deodorant.
- A guide to the Breast Screening (mammogram) appointment for the Deaf Community created by the Dudley, Wolverhampton and South West Staffordshire Breast Screening Programme
What having a mammogram feels like
Having a mammogram can be uncomfortable, and some women find it painful. Usually, any pain passes quickly.
Please contact your breast screening unit before coming for your appointment if you:
- need information in another format
- need additional support to attend screening, for example if you have a learning disability or mobility problems
- have breast implants
- have a pacemaker or any other implanted medical device
- are pregnant or breastfeeding
- are under the care of a breast consultant
- have had a mammogram in the last 6 months
Breast screening results
You will receive a letter with your breast screening results within 2 weeks of your appointment. The results will also be sent to your GP.
Occasionally women will need another mammogram before they get their result. Sometimes technical problems mean that the mammogram is not clear enough to read. If this happens, you will be asked to have another mammogram to get a clearer picture of your breast.
Most women will have no sign of cancer
In about 96 out of every 100 women screened the mammogram will show no sign of cancer, and no further tests are needed.
Cancer can still develop between mammograms. Remember to check your breasts and tell your GP straight away if you notice any unusual changes.
Some women will need more tests
The results letter may say you need more tests because the mammogram looks abnormal. About 4 in every 100 women are asked to come back for more tests after screening.
Out of these 4 women, 1 will be found to have cancer. The rest will not have cancer and will go back to having screening invitations every 3 years.
If you are called back for more tests, you may have a breast examination, more mammograms and ultrasound scans. You may also have a biopsy, which is when a small sample is taken from your breast with a needle to be checked under a microscope. You will usually get your results within a week.
If you are found to have breast cancer, it could be either non-invasive or invasive
Non-invasive breast cancer
About 1 in 5 women diagnosed with breast cancer through screening will have non-invasive cancer. This means there are cancer cells in the breast, but they are only found inside the milk ducts (tubes) and have not spread any further. This is also called ductal carcinoma in situ (DCIS). In some women, the cancer cells stay inside the ducts. But in others they will grow into (invade) the surrounding breast in the future.
Doctors cannot tell whether non-invasive breast cancers will grow into the surrounding breast or not.
Invasive breast cancer
About 4 in 5 women diagnosed with breast cancer through screening will have invasive cancer. This is cancer that has grown out of the milk ducts and into the surrounding breast. Most invasive breast cancers will spread to other parts of the body if left untreated.
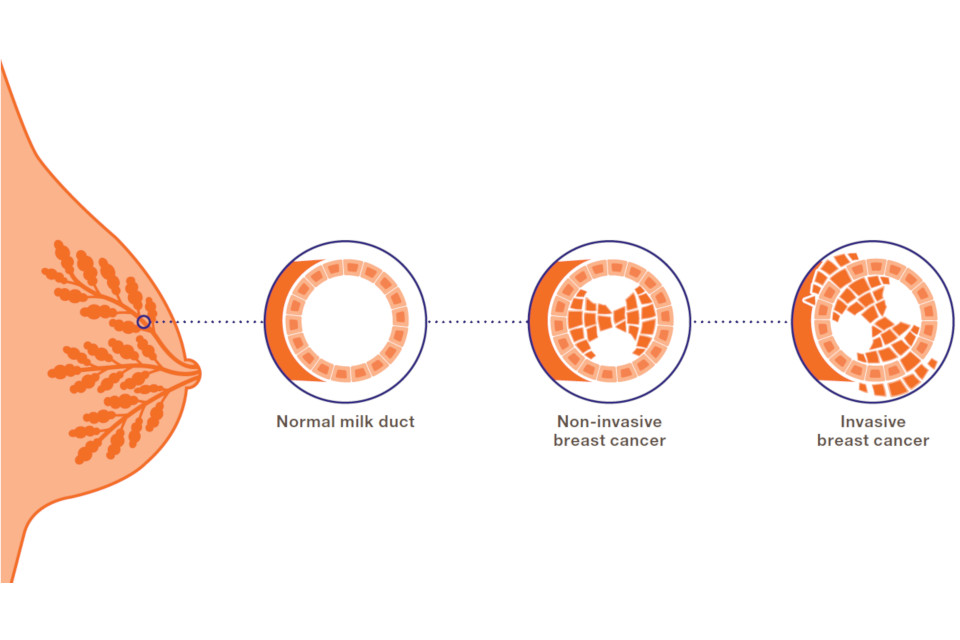
Diagram showing the development of breast cancer in a milk duct
Breast cancer treatment
Whether the cancer is invasive or non-invasive, you will be offered treatment and care from a team of breast cancer specialists. The treatment is likely to include surgery (which may mean a mastectomy), radiotherapy, hormone therapy and possibly chemotherapy. These treatments can cause long-term side effects.
Making a choice: the possible benefits and risks of breast screening
It is your choice whether or not you have breast screening. There are many different reasons why women decide whether or not to have screening. To help you decide, we have included information on the possible benefits and risks.
Screening saves lives from breast cancer.
Lives are saved because cancers are diagnosed and treated earlier than they would have been without screening.
Screening finds breast cancers that would never have caused a woman harm.
Some women will be diagnosed and treated for breast cancer that would never otherwise have been found and would not have become life-threatening. This is the main risk of screening.
Doctors cannot always tell whether a breast cancer that is diagnosed will go on to be life-threatening or not, so they offer treatment to all women with breast cancer. This means that some women will be offered treatment that they do not need.
Weighing up the possible benefits and risks of breast screening
There is debate about how many lives are saved by breast screening and how many women are diagnosed with cancers that would never have become life-threatening. The numbers below are the best estimates from a group of experts who have reviewed the evidence.
Saving lives from breast cancer
Screening saves about 1 life from breast cancer for every 200 women who are screened. This adds up to about 1,300 lives saved from breast cancer each year in the UK.
Finding cancers that would never have caused a woman harm
About 3 in every 200 women screened every 3 years from the age of 50 up to their 71st birthday are diagnosed with a cancer that would never have been found without screening and would never have become life-threatening. This adds up to about 4,000 women each year in the UK who are offered treatment they did not need.
Overall, for every 1 woman who has her life saved from breast cancer, about 3 women are diagnosed with a cancer that would never have become life-threatening.
Researchers are trying to find better ways to tell which women have breast cancers that will be life-threatening and which women have cancers that will not.
Other risks of breast screening
Most women who need more tests after breast screening are found not to have breast cancer. These women experience unnecessary worry and some feel distress which affects their ability to do their normal day-to-day activities at the time.
X-rays can very rarely cause cancer. Having mammograms every 3 years for 20 years very slightly increases the chance of getting cancer over a woman’s lifetime.
Mammograms do not find all cancers. Sometimes they cannot be seen on the mammogram, and very occasionally mammogram readers will miss a cancer on the X-ray. Your breasts may change between screening appointments so it is important to check your breasts regularly to know what is normal for you. Please talk to your GP if you have any concerns.
Symptoms of breast cancer
If you get to know how your breasts normally look and feel, you will be more likely to spot any changes that could be signs of breast cancer. This is important even if you have been for breast screening. Look out for:
- a lump or thickening in the breast
- a swelling or lump in the armpit
- a change in the nipple, which might be pulled back into the breast, or change shape – you might have a rash that makes the nipple look red and scaly, or have blood or another fluid coming from the nipple
- a change in how the breast feels or looks – it may feel heavy, warm or uneven, or the skin may look dimpled; the size and shape of the breast may change
- pain or discomfort in the breast or armpit
If you have any change to your breast, you should make an appointment to see your GP straight away. You may not have cancer. But if you do, being diagnosed and treated at an early stage may mean you are more likely to survive breast cancer.
What happens to your mammograms after screening
The NHS Breast Screening Programme will keep your mammograms for at least 8 years. These are saved securely. The programme regularly checks records to make sure the service is as good as possible. Staff in other parts of the health service may need to see your records for this, but your records will only be shared with people who need to see them.
We will review your previous screening results if you are diagnosed with breast cancer between screening appointments. You can see the results of this review if you wish.
Confidentiality
The NHS screening programmes use personal information from your NHS records to invite you for screening at the right time. Public Health England also uses your information to ensure you receive high quality care and to improve the screening programmes. Find out more about how your information is used and protected, and your options.
More information
If you have questions about screening, please contact your local breast screening unit.
If you would like to talk to someone about whether to have breast screening, your GP can help. Together, you can weigh up the possible benefits and risks, to help you decide.
Information about breast screening can be found on the NHS website, including details of your local breast screening unit.
Find out how to opt out of breast screening.
 Breast Screening is offered to all eligible women registered with a GP routinely every 3 years between the ages of 50 - 71.
Breast Screening is offered to all eligible women registered with a GP routinely every 3 years between the ages of 50 - 71.
Every woman will receive their first invite before their 53rd birthday, and then 3 yearly from the date of their first screening.
Our information is compiled from GP records, so it is important to make sure your details are correct.
If you are over 71 and have not been screened in 3 years you are also welcome to contact our office on 01524 518699 to make an appointment.
The aim of breast screening is to detect breast cancer at an earlier stage, often before the woman is aware of any problem. Scientific evidence shows that regular breast screening, between the ages of 50 - 71 years, reduces the death rate from breast cancer.
80% of breast cancers occur in women over 50. The risk of breast cancer rises as women get older, which is why the breast screening programme only targets women in this age group.
We have a range of screening locations to choose from. We will aim to offer you a screening appointment at a location closest to you, when you contact us However, this may not always be possible, based on demand and the location of our screening mobiles at that time.
- Westmorland General Hospital - Kendal
- Furness General Hospital - Barrow-in-Furness
- Royal Lancaster Infirmary - Lancaster
- Mobile vans provide a screening service across Blackpool and Fylde and Wyre areas, which visit car parks at:
If you require the directions or maps in a more accessible format, please contact communications.team@mbht.nhs.uk
Your mammograms (x-ray) are reviewed and the results will normally be sent to you within two weeks. Your GP will also be notified of your results.
There are 3 possible results:
1. Normal
Your x-rays have shown no signs of cancer and you will be invited again in 3 years time for your next routine screen. If you will be over 70 then please contact us for an appointment nearer the time.
2. Technical Repeat
The mammogram needs to be repeated for technical reasons only. The quality of the x-ray does not allow for all the breast tissue to be seen clearly. Approximately 3 out of every 100 women screened will be called back for a technical repeat to get a good quality mammogram.
3. Assessment
Sometimes the mammograms do not give enough information and a further examination is needed before we can decide on a result. If this is the case you will receive an appointment to attend our assessment clinic at the Royal Lancaster Infirmary Breast Care Unit. This additional appointment is part of routine screening and for most women invited back nothing of concern will be found. Any women invited to an assessment clinic will be able to speak to a breast care nurse if they want more information before attending.
You have been invited back for further tests because your breast x-rays did not give us enough information and more detail is needed before we can decide on a result.
If the clinician interpreting the screening mammogram images sees something that is questionable, unclear or abnormal on the images, they ask the patient to come back for further assessment.
This additional appointment is part of routine screening and for most women invited back nothing of concern will be found.
On arrival most women will meet a Radiographer or Radiologist who will explain what is to happen during the clinic.
You may have some or all of the following tests:
- Breast examination: the doctor / practitioner will talk to you about your mammograms, will ask you some questions about your general health and will then examine your breasts.
- Mammogram: most women will have further mammograms in order to show a particular part of the breast in greater detail.
- Breast ultrasound: ultrasound will be necessary for all women. An ultrasound scan uses sound waves to provide a picture of the breast tissue. It is harmless and pain free and does not involve any x-rays
- Breast needle biopsy: it may be necessary for some women to have a small tissue sample taken from the breast. Local anaesthetic is always used to numb the area first.
Before you leave the clinic the Radiologist will talk to you about your results. In most cases, the Radiologist will tell you the results of the tests on the same visit. If a needle sample is taken, the breast care staff will make an appointment for you to receive your results.
Change your appointment
If you are unable to attend your allocated breast screening appointment detailed in your letter, or if you wish to cancel the appointment, please fill in the form below using the details from your letter and we'll contact you in writing within 14 working days with a new appointment date.
Frequently asked questions
Female breast cancer self-examination video
Male breast cancer self-examination video
How to be breast aware | An information video for the Deaf Community created by the Dudley, Wolverhampton and South West Staffordshire Breast Screening Programme
Yes, please complete the online form to request an alternative date, time or location of your screening appointment.
Alternatively you can call the screening office on 01524 518699 (9am - 4pm, Monday - Friday).
 Having a mammogram can be uncomfortable and some women find it painful. Usually, any pain passes quickly.
Having a mammogram can be uncomfortable and some women find it painful. Usually, any pain passes quickly.
We respect your decision not to be screened, although we would encourage all women to attend their breast screening appointment when invited. However, if you choose not to take up your invitation please contact the screening office to inform us that you do not wish to take up the invitation.
If you change your mind, ideally within six months of receiving your invite, we will be happy to arrange screening for you.
Where possible, please attend your appointment alone. Please be aware that there is limited space at some of our screening sites, particularly the mobile screening vans.
We would discourage anyone to bring young children with them. The mammograms use x-rays so no one else can be present in the x-ray room so your children would have to sit in the waiting room by themselves.
Men may be present in the main waiting area, but a female Mammographer will always perform the x-ray.
Please contact the screening unit using the online form and we will arrange a new appointment for you.
You will be asked to undress completely down to your waist so it is a good idea to wear a separate top instead of a dress.
Some deodorants and talc are visible on the mammograms and can lead to the mammograms being repeated so it is best not to wear any deodorant or talc. You can always bring some wipes and wipe any deodorant off before your appointment.
No. Breast screening aims to find breast cancer at an early stage when it may be too small for you or your doctor to feel. Finding breast cancer early greatly increases the chance of successful treatment
Please contact us on 01524 518699 to discuss your screening appointment for us to establish if this invitation is suitable for you to attend.
If you have a breast lump or any other breast symptoms you should make an appointment with your GP, who can organise a referral to your local breast unit.
Any x-ray involves radiation, but mammograms only require a very low dose. It is about the same as the dose a person receives by flying from London to Australia and back. The risk that such a low dose could cause a cancer is far outweighed by the benefits of early detection of breast cancer.
Your results will be sent to your home address and you should expect to receive them within 2-3 weeks. You will be advised of any expected delays at the time of your screening.
A female Mammographer will always perform the x-ray.
Yes, it is safe for you to have a mammogram. It is helpful if you can tell the Mammographer where your pacemaker is sited.
Breast implants appear as a solid white area on a mammogram. This may hide some of the breast tissue preventing it from being seen on the x-ray. The film readers will only be able to report on the breast tissue that they can see on your mammogram so usually extra images are taken. Before commencing the mammograms, the Radiographer will explain everything to you so that you will be aware how your mammograms will differ to mammograms without implants.
Please contact us on 01524 518699 to discuss your screening appointment, as we would like to allocate more time for your appointment. Your appointment will be made at one of our units in Barrow, Kendal or Lancaster where we have larger rooms and disabled access.
Breast Screening Unit
Ashton Court
Royal Lancaster Infirmary
Lancaster
Lancashire
LA1 4RP
Tel: 01524 518699 (9am - 4pm, Monday - Friday)
Email: bsu.rli@mbht.nhs.uk


