You have now been added to the list for elective surgery
What happens next?
Following the outpatient appointment:
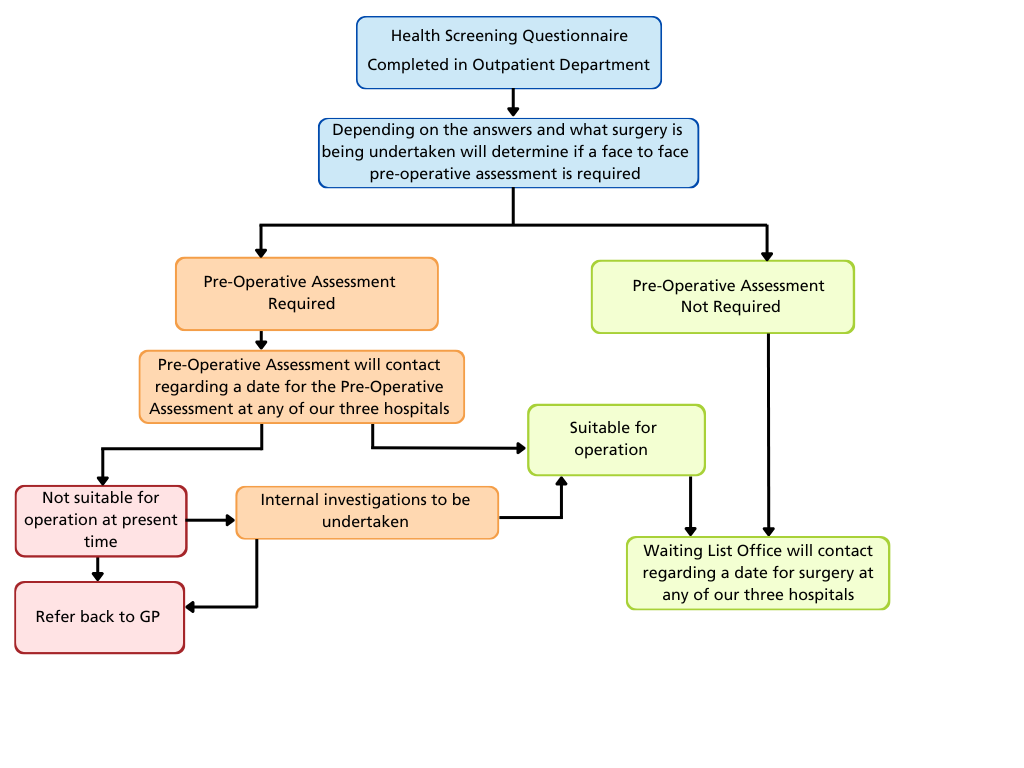
The health screening questionnaire (HSQ) that you have completed will determine whether you will be asked to attend for a pre-operative assessment or not. This appointment could take place at any of the three main hospitals:
Royal Lancaster Infirmary (RLI - Lancaster), Westmorland General Hospital (WGH - Kendal), Furness General Hospital (FGH - Barrow).
Pre-operative assessment team telephone numbers:
Furness General Hospital: telephone 01229 404491
(Office hours - Monday - Friday 8:30am - 4:30pm)
- Royal Lancaster Infirmary 01524 512117
- (Office hours - Monday - Friday 8:30am - 4:30pm)
- Westmorland General Hospital 01539 715767
- (Office hours - Monday - Friday 8:30am - 4:30pm)
There is an answerphone service.
Your surgery will take place at the hospital that is most appropriate for your needs and is dependent on a number of factors.
- It is your responsibility to inform us if you are unable to attend any arranged appointment in a timely manner, to enable us to reallocate your appointment.
- Please make sure you will be available for the next 18 weeks.
- If you are planning a holiday for two or more weeks, or have other commitments, please inform the pre-operative assessment team when they contact you.
- If you make yourself unavailable for any length of time, following a clinical review this could result in you being discharged back to your GP.
- Please inform the waiting list office of any change of address or telephone number (landline and / or mobile) to ensure we can contact you
- Not attending for your operation could cost the NHS between £1500 and £5000, if we were unable to reallocate your time slot to someone else.
Please ensure you read the letters carefully as we operate at three hospitals.
Pre-Operative Assessment
At pre-operative assessment you will have a test appointment were your blood pressure, pulse, height and weight will be checked. You may have an ECG (electrocardiogram) which takes a tracing of your heartbeat, and some bloods may be taken. A nurse will also listen to your heart and lungs and examine your mouth and airway.
A second POA appointment either on the same day, if its face to face, or the following day, if the appointment is via the telephone, will also be made for you. The nurse at this second appointment will follow up on the test results, go through your past medical and surgical history, identifying any issues or conditions that may need to be optimised. If any issues are identified you will either be referred to see an anaesthetist, be referred to other specialists for input or referred to your GP. If everything is satisfactory the nurse will pass you fit to proceed to surgery.
Once you have passed your pre-operative assessment, waiting list office will be informed and your surgery will be planned at the most appropriate site for your surgery. You will be contacted directly by waiting list office team once a date has become available for your surgery.
Once this date has been agreed, it is important that you inform us of any changes to any of the below, by contacting the pre-operative assessment team:
Medications
- Any recent infections - on your skin, chest, or urine
- New illness / diagnosis
- Admission to hospital for a different condition
- Worsening of known chronic medical conditions
- Please let us know in plenty of time if you are unable to attend an appointment
If you do not inform us of such changes, this could lead to cancellation of your surgery on the proposed day.
Please take note if you have been given instructions regarding your medications following your pre-operative assessment
It is very important that you also contact us if your condition has significantly improved and you don’t feel you require the surgery any more.
Attending your appointment
If you do not attend (DNA):
It is very important to give us prior notice if you are unable to attend an appointment. Nine out of ten patients arrive on time for their appointments. However, even one missed appointment can cause delays for you and other patients, and waste precious NHS resources.
If you miss your appointment and don’t let us know in advance you are at risk of being referred back to your GP.
If you are unavailable:
If your treatment is routine please make sure you will be available for the next 18 weeks. If you are unavailable for personal reasons for an extended period of time, e.g. six weeks or longer, then we refer your case to your consultant for a clinical decision on the next step. Extending the time before we can give you your treatment by making yourself unavailable could lead to your condition worsening.
If you are unfit:
If the clinical issue is short-term (e.g. cough, cold) and has no impact on the original clinical decision to undertake the procedure we will wait until you have recovered before giving you a new date.
For longer term illnesses, if the clinical issue is more serious and you require investigations or treatment for it, clinicians will make a decision to either:
Remove you from the waiting list and see you again in clinic in a set period of time, (for example, six months).
or
Discharge you back to the care of your GP so that they can optimise/ treat your illness first. When you are fit, you will be re-referred for treatment.
Every year patients who do not attend for their surgery increases the financial burden on the NHS, as well as increasing waiting times for all patients.
What you will need when you come into hospital for a planned operation or treatment:
- Bring any drugs, medicines or inhalers you are using in their original boxes. Bring an up to date prescription if you don’t have the boxes
- Nightdress/pyjamas, dressing gown and slippers to preserve your dignity when walking to theatre (this does not mean you will be staying overnight as you may be discharged later that day.)
- Toiletries
- Towels if a planned overnight stay
- Wear loose, comfortable day clothing
- Books, magazines, stationery etc.
- Please bring minimal belongings with you
- The telephone number of whoever is collecting you from the hospital
- Wear glasses rather than contact lenses
- Credit / Debit card if you want to order a TV at RLI / FGH
- Phones for personal music with ear phones. Please be considerate when making telephone calls.
Do not bring:
- Large amounts of money
- Jewellery, other than a wedding ring. Please remove any body
- jewellery or piercings
- Please do not wear or bring heavy makeup, nail polish or acrylic /
- synthetic or any other type of false nails
- Aerosols - as these can set off the fire alarm
- Pets
Preparing For Your Operation
If you are having a general or spinal anaesthetic or having sedation, please follow the instructions below:
Morning operation:
- To reduce the risk of complications from the general anaesthetic you should not eat for six hours before your arrival time. This includes chewing gum and sweets, and drinks containing milk.
- In order to aid your recovery we suggest that you have a drink between 1/2 and 1 pint of still tap water before 6:30am and take any regular medication at this time unless advised otherwise.
Afternoon operation
- You should have a light breakfast (for example cereal or a slice of toast) no later than 7.30am
- We advise you drink water between 7.30am and 11.00am to aid your recovery.
- You should take any regular medication as usual on the morning of your operation, unless advised otherwise by surgeon or pre-op assessment.
If you take any medication this should have been discussed with you beforehand, but if you have any questions please call the pre-operative assessment team.
If you are NOT having a general anaesthetic then please only have a light breakfast (for example, a slice of toast) / lunch (such as a sandwich) prior to arrival.
You can continue drinking all non-alcoholic fluids up to your admission.
If you are having a procedure on the hand/arm on which you wear your wedding ring, please could you remove it before arrival.
Please help us to help you:
- Please bath / shower on the day of your operation / admission.
- Please do not shave, clip, or wax around the area where your surgery is to
- be performed.
- Staying warm before surgery will lower the risk of postoperative complications.
- The hospital environment may be colder then your own home, so please
- bring additional clothing to help keep you comfortably warm. Please tell staff if you feel cold at any time during your hospital stay.
Please note:
- There are no facilities for relatives to stay on the ward or wait in the admission areas but there are canteen facilities available on all three sites.
- While you are a patient in one of our hospitals, please ensure you maintain good hand hygiene throughout your stay.
- Please do not sit on other patient’s beds or chairs and ensure any visitors you may have use the chairs available.
- Please remind your visitors to use the alcohol gel or hand washing facilities on entrance and exit to all wards and departments.
- All our staff are trained in the importance of hand hygiene, but if you haven’t seen a member of staff clean their hands when you think that they should have done, please feel free to ask them to do it again. No offence will be taken.
- Smokers are advised not to smoke 12 hours before admission.
- We have a no smoking policy throughout the hospital and the grounds. The stop smoking service can be contacted on the NHS North Lancashire: 01524 845145 or NHS Cumbria: 01900 324222.
What Will Happen on the Day of Your Operation?
Please report to the department / ward reception desk, where indicated on your letter. A registered nurse will be allocated to coordinate your nursing care throughout your stay.
You will be asked for any relevant personal information, including contact details in case of an emergency.
You will be required to wear an identity bracelet at all times. Equally, all staff wear ID badges.
There is a bedside cabinet for your day to day needs and personal belongings.
The majority of the bedsides across our hospitals (except Westmorland General Hospital) have their own touch screen entertainment unit that includes TV, phone, internet, and film on demand. For more information on the units, please visit:
http://www.hospedia.co.uk/patients-and-visitors.html
(Please note that University Hospitals of Morecambe Bay Foundation Trust is not responsible for the content of this external website)
Free WiFi is available throughout our hospital sites.
You will meet the surgeon and the anaesthetist prior to your surgery. You will find that you are asked the same question more than once; this is all part of a careful checking system.
As operating sessions normally run between approx. 8.30-12.30pm and 1.30- 5.30pm you may have to wait for some time for your operation. The time given in your letter is the time of your admission; it does not mean your surgery will be straight after this, as you may not be the only person having surgery for that session.
Your named nurse for that day will keep you updated as to the time of your operation.
You’ll be asked to change into a hospital gown. You can also wear your slippers and dressing gown, as you will be asked to walk to theatre or go in a wheel chair rather than on a trolley.
Occasionally you may need a needle connected to a drip which will be inserted into your hand, allowing fluids, nourishment and medicine to be given during your recovery.
If you have had a general anaesthetic or sedation, you will wake in the recovery area and then be taken back to the ward. Some degree of soreness and drowsiness is expected.
We will do our utmost for your surgery to go ahead on the day planned, but there may be instances when there may be last minute cancellations. Examples may be:
- Bed unavailability
- Emergency patients requiring the theatre space
- Staff sickness
- Complications from previous patients on your list
Following Your Operation:
Pain relief after your operation
Pain relief may be given before, during and/or after the operation. This may be by tablet, suppository or injection. Local anaesthetic may be placed around the operation site which may stay numb for several hours. As this wears off, you may experience some pain, so take the pain relief regularly as instructed.
It would be useful to ensure you have a supply of your usual pain relief at home, such as paracetamol or ibuprofen, which can be bought from a chemist. You may be given further pain relief to take home with you, but this will be explained on discharge. Ensure you follow dosage guidelines at all times. Do not exceed maximum daily doses.
Avoiding blood clots
Staying mobile in hospital can help you recover more quickly. Being immobile can lead to additional health problems, such as infections and pressure sores. It can also increase your risk of venous thromboembolism (VTE), which is when a blood clot forms in a vein.
To avoid VTE, you will be encouraged to move about the ward regularly. You will be given as much assistance as you need to move about. If you’re at an increased risk of VTE, you may be given compression stockings to improve your circulation, or given medication as a precaution.
Discharge:
Before you leave the hospital you may (depending on the type of operation you’ve had) have an appointment with a physiotherapist, who will be able to advise you about any exercises you need to carry out.
You’ll also be given advice about how to care for your wound, and any equipment you may require, such as dressings, bandages, crutches and splints.
Your discharge will be affected by:
- how quickly your health improves while you’re in hospital.
- what support you’ll need after you return home.
You will be informed if you require a follow-up appointment that will be sent through the post.
General Information
During Your Stay
- Smoking or vaping is not permitted on any of the hospital sites. If you are a smoker you are to avoid smoking for 12 hours before your operation.
- Please be considerate when making telephone calls. Mobile devices are restricted in areas of the Trust premises to preserve privacy and dignity of all persons, especially where their use may disturb or disrupt others or cause an issue with medical devices. Areas where restrictions apply will have signage which shows the type of restriction (either mobile device turned off or set to silent). All persons within the area are asked to comply.
- There is a bedside cabinet, but these are not locked. The staff will go through a property disclaimer with you on arrival to hospital relating to liability and personal possessions.
Going Home
- A responsible adult must take you home by car / taxi. You must not drive yourself, or use public transport, unless accompanied, after an operation.
- If we have planned for you to go home the same day as your surgery, it is your responsibility to arrange for a responsible adult to be at home with you for 24 hours after your operation. There will be some instances where you will be allowed to go home alone, however the criteria is very tight and this won’t be known until after your surgery.
- It is more advisable to make sure you have someone able to stay with you after a general anaesthetic. If you have a day case procedure and are not staying overnight, you may be discharged into the evening, depending on your recovery and position on the theatre list.
-
Whoever is collecting you can contact the ward following your surgery to arrange a suitable time to collect you.
If we have planned for you to stay overnight, you will be informed the day before your planned discharge that we will aim for you to be ready to be discharged from your ward by 10am the following day.
For 24 hours after your operation /anaesthesia:
- Do not drive or ride a bike. This may be for longer depending on the procedure you have, you will be advised about this by the surgeon.
- Do not operate any machinery (including a cooker) or do anything requiring skill or judgement.
- Do not smoke or drink alcohol.
- Do not take sleeping tablets.
- Do observe any special instructions we may give you.
Additional Useful Information:
Enquiries:
Switchboard for all inpatient hospitals: 01539 732288
Pre-operative assessment team telephone numbers:
Furness General Hospital: 01229 404491
Royal Lancaster Infirmary: 01524 512117
Westmorland General Hospital: 01539 715767
Waiting list office telephone number:
Royal Lancaster Infirmary: 01524 516311
Furness General Hospital: 01229 403644
Day surgery ward telephone numbers:
Furness General Hospital: 01229 491081
Westmorland General Hospital: 01539 795205.
Visiting
Visitors should be limited to two per bed at any one time. There may be times when visiting is restricted due to infection outbreaks, but you will be informed of this by the ward staff. Please also note, visiting hours are different on some wards so please check before visiting.
Please ask that anyone who is suffering or recovering from an infectious illness, such as diarrhoea, vomiting, coughs or colds, refrains from visiting you.
Day Surgery areas for all sites
The ward staff will inform you of a suitable time to call back to collect your relative / friend. This may be into the evening even up to 11pm which helps to create beds for admissions the next morning.
Patient Information
Hospital Passports – Adult and Child are on our website
https://www.uhmb.nhs.uk/patients-and-visitors/coming-intohospital/ hospital-passport
Condition specific information leaflets:
The Trust has a collection of approved patient information leaflets available on the website, both from the Trust and external sources. It can be accessed under ‘Our Services - Patient Information Leaflets’, or at the address below:
https://www.uhmb.nhs.uk/document-library
Additional information for a wide range of conditions can be found on the NHS Choices website:
http://www.nhs.uk/pages/home.aspx
Interpreters can be arranged at a patient’s request. Please contact the department as far in advance of your admission as possible to ask them to arrange this.
Anaesthetic Information: visit www.rcoa.ac.uk/patientinfo
Frequently Asked Questions:
What time will I be allowed home?
If you are required to stay overnight, we aim for you to be discharged by 10am. If you are a day surgery patient, you may be discharged up until 11pm that evening.
Will I see the surgeon before I go home?
Not necessarily, as we are a multi-site Trust. However, you will receive appropriate post-operative instructions.
Is there anything I should avoid doing?
Please refer to the section During Your Stay. If there is anything else the staff will inform you of this on discharge.
How long will it take me to recover and get back to normal?
This will be dependent on the type of operation you have had, but staff will ensure you are aware of this information on discharge.
Am I allowed to smoke?
No, the Trust complies with a no smoking policy.
Who will look after me when I get home?
It is your responsibility to find a suitable adult to stay with you for the initial 24 hours following a general anaesthetic, unless you fit the tight criteria to be discharged home alone. There could be a risk that if you do not have anyone to stay with you and you need someone, your surgery may be cancelled due to bed availability.
Will I be given any pain relief on discharge?
Instructions and appropriate advice will be given to you by the nurse who discharges you. Please make sure you have a supply of your usual pain relief including paracetamol and ibuprofen
Who will arrange my transport?
There is a strict criteria for hospital transport, otherwise it is your responsibility to arrange your own transport home.
Please visit http://www.nwas.nhs.uk/our-services/patient-transport-service/ for more details.
Key Information on Attending Appointments at UHMBT
As per the NHS Constitution, all patients have the right to access consultant-led services within 18 weeks and also the right to choose which hospital trust they wish to have their appointment and any subsequent treatment at.
Here at UHMBT, we offer consultant-led care at:
- Furness General Hospital in Barrow
- Royal Lancaster Infirmary
- Westmorland General Hospital in Kendal
- Ulverston Community Health Centre
- Queen Victoria Hospital in Morecambe
If you choose to have your appointment at UHMBT, we will offer you the first available appointment, depending on clinical need, at the most appropriate site for your treatment. Please note that this may not be the hospital nearest to where you live.
If you have difficulty travelling to your appointment, you may be able to access patient transport.
More information on this can be found at: http://www.nwas.nhs.uk/our-services/patient-transport-service/
Publication date: 14/07/2022
Review date: 01/07/2025
Leaflet code: UHMB-FT090/PIL095

