Patient Safety Incident Investigation Guide
What to expect and how you can be involved in the process
About this guide
Why am I receiving this guide?
We are very sorry that you, your friend/family member, or the person you care for, has been involved in an incident in our Trust. You are receiving this guide because we are going to carry out an investigation.
A Patient Safety Incident Investigation (PSII) is something an NHS Trust does to learn about what happened, why it happened, and what can be done to make sure that it doesn’t happen again.
We would like you to be part of the investigation process as much as you would like to or feel able to. This guide has been designed to explain the investigation process, how you can be involved, and what to expect. It is okay if you do not want to be involved. It is also okay if you change your mind about your involvement at any time throughout the investigation.
You can ask your Engagement Lead for paper copies.
Patient safety incidents in the NHS
Patient safety incidents are unintended or unexpected events in healthcare that could have or did cause harm to one or more patients. The Patient Safety Incident Response Framework (PSIRF) was written as a guide for all NHS trusts in England on how to identify and respond to patient safety incidents.
If you would like to know more about PSIRF you can find it here:
www.england.nhs.uk/patient-safety/patient-safety-insight/incident-response-framework
We have written our own plan based on this national document; you can find it here:
www.uhmb.nhs.uk/our-trust/patient-safety-incident-response-plan
A patient safety incident is a type of patient safety event that is reportable so you may hear both terms. In our Trust, we more commonly use the term patient safety event.
There are different words or phrases to describe types of patient safety event, for example:
- Adverse event.
- Near miss.
- Never event.
The introduction of PSIRF gives NHS Trusts different ways to respond to patient safety incidents. The different responses are explained in the PSIRF plan. The responses include investigations and other ‘Learning Responses’ (ways of learning from patient safety incidents).
In your case, we (University Hospitals of Morecambe Bay NHS Trust), have decided to undertake a Patient Safety Incident Investigation (PSII), as what has happened indicates a significant safety risk and there is potential to prevent this happening again, by learning and changing.
Patient Safety Incident Investigations (PSII)
What is a Patient Safety Incident Investigation?
Patient Safety Incident Investigations (PSII) are undertaken to identify what has happened and how it can be prevented from happening again, by learning and improving.
The aim of a Patient Safety Incident Investigation is to understand:
- What happened.
- When did it happen.
- Why did it happen.
- What contributed to it happening.
- What can be learned.
- How the Trust can share the learning.
- How the Trust can prevent something similar happening again.
Incidents are very rarely caused by a single thing; usually there are multiple reasons. The investigation will aim to establish the facts, identify procedures, practices, and areas in the care system or organisation that might need to be changed or improved. It is not to apportion blame, but to capture learning opportunities. The investigation will begin as soon as possible after the incident has occurred and will normally be completed within three to six months. The timeframe can be extended with agreement of those affected, including patients, families, carers, and staff.
The investigation will be carried out by a named Learning Response Lead who is experienced and trained to carry out investigations for learning. The Learning Response Lead will be someone who has seniority and experience within the Trust and who has the dedicated time to carry out the investigation. We will make sure that the Learning Response Lead will be someone who was not directly involved in what happened.
What process does a Patient Safety Incident Investigation follow?
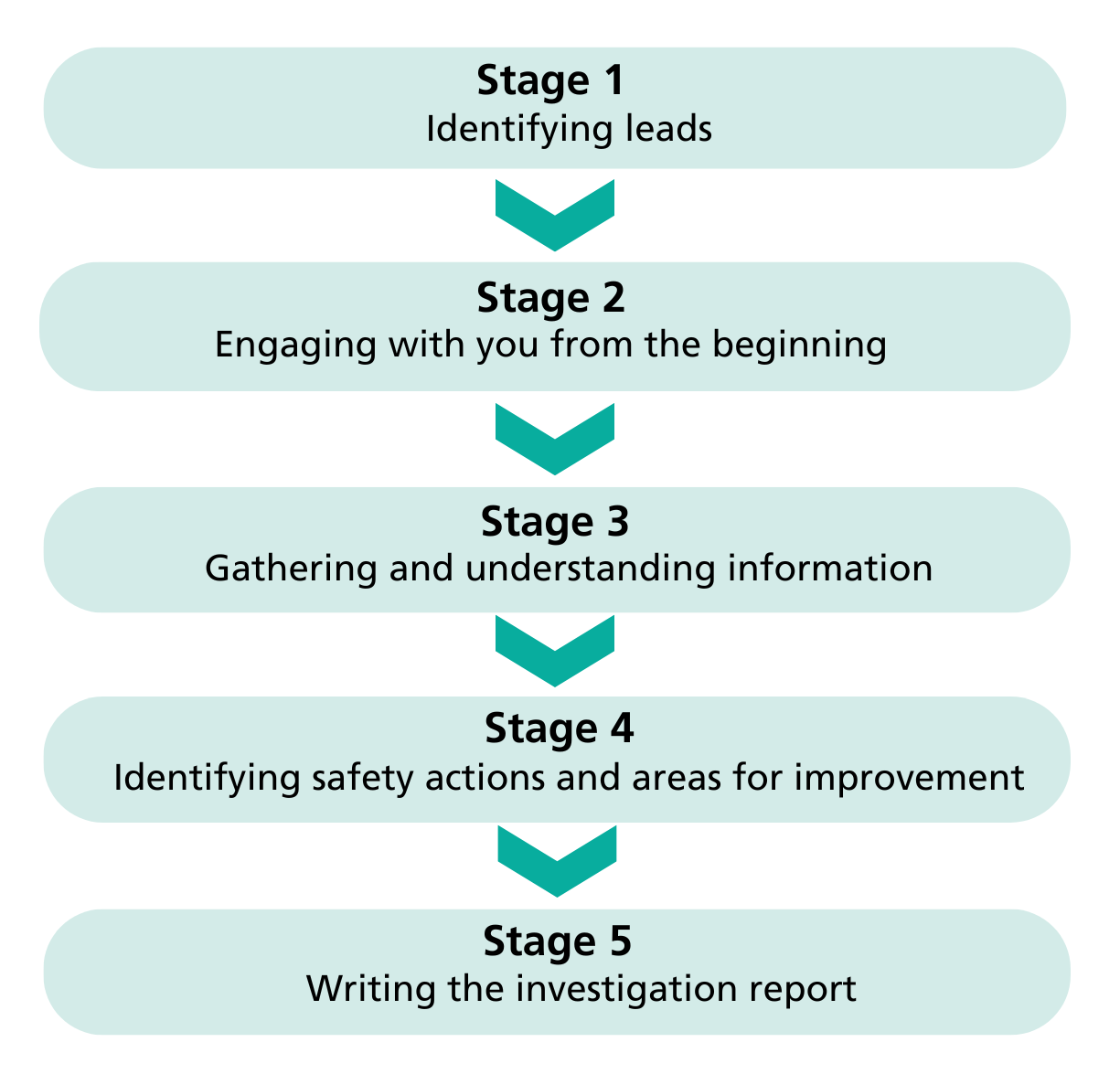
Your investigation stage 1: identifying leads.
- The investigation will start as soon as possible.
- We will identify a trained and independent Learning Response Lead to carry out the investigation.
- We will identify an Engagement Lead to liaise with you throughout the investigation.
- Your Engagement Lead will be your main point of contact.
Once known, you might find it helpful to record their details as below:
- My Engagement Lead
- Their email address
- Their telephone number
- Their working hours are/the best time to contact them
There may be other people that you have as a point of contact, such as:
- Patient Safety Specialist.
- Patient Safety Partners.
Their individual contact details will be given to you by your Engagement Lead should you require them.
Your investigation stage 2: engaging with you from the beginning.
Your Engagement Lead will contact you to introduce themselves and listen to your experience as it will help us to compile a picture of what happened. They will explain the investigation process and ask how involved you would like to be, and what you want from the investigation. Your Engagement Lead will work with you in a compassionate way.
During the investigation, your Engagement Lead will be able to answer your questions about the investigation progress, supporting you to understand what is happening and helping you to be as involved as you would like/are able to be.
The Learning Response Lead will set the terms of reference for the investigation and will include your requests that you have shared at this point. Terms of reference will cover aspects of care that the investigation will look at, with agreed boundaries - what is included and excluded from the investigation. With your agreement, you will help to set the terms of reference as you may have your own questions that you want to be answered; you can discuss this with your Engagement Lead.
You may need time to think about questions and you will have time to do this as they can be incorporated at any time. It is okay if you do not have any questions, or do not want to be involved in the investigation process at all. The investigation will continue no matter your level of involvement, as it is important for the Trust to learn and make improvements.
You can read more about engaging and involving patients and families here:
www.england.nhs.uk/publication/patient-safety-incident-response-framework-and-supporting-guidance
Terms of reference – agreeing how we work together
You may like to write down the terms of reference for your investigation.
The following prompts may help you to create questions you would like included in the terms of reference.
- How would you describe what happened?
- How has what happened affected you, and those around you?
- What do you need to support you and your family following what happened?
- What questions do you have about what happened?
- What would you like to see happen next?
Your investigation stage 3: gathering and understanding information.
As well as listening to your experience, there are lots of different types of information the Learning Response Lead will gather to answer the questions set out in the terms of reference. They:
- will look at medical, nursing and care records to see what was written down.
- will talk to people involved to understand what happened.
- will visit the area to observe the environment and how people work.
- will read policies and guidance to understand what should have happened.
- may search for common themes, carry out a risk analysis, or may need to gather more information from other sources.
Once all the information has been gathered, the Learning Response Lead will analyse the information. There are recommended frameworks and structures that will be used to make an informed judgement (this is making a judgement
from the information gathered).
We use a framework called System Engineering Initiative for Patient Safety (SEIPS); it’s a way to understand how healthcare works as a system. The key idea is that patient safety depends not just on individual doctors or nurses or other staff, but on how well the whole ‘system’ functions. SEIPS looks at how all these parts work together to make it easier to identify problems and ways to make the whole system safer and more effective for patients by improving how it all works together.
This system includes:
- People: everyone involved in providing care, like doctors, nurses, and patients.
- Tools and technology: machines, computers, and devices used to treat or keep track of patients’ health information.
- Tasks: the jobs people must do, like giving medications or updating medical records.
- Environment: the physical space, like the hospital or clinic where care is provided.
- Organisation: includes the policies, teamwork, and leadership that keep everything running smoothly.
You can read more about SEIPS here:
www.england.nhs.uk/publication/patient-safety-learning-response-toolkit
Your investigation stage 4: identifying safety actions and areas for improvement
Once the Learning Response Lead has analysed the information, they will identify immediate safety actions and areas for improvement to stop or reduce the likelihood of something similar happening again. Areas of improvement will be addressed as part of a Quality Improvement Project (QIP). We welcome your contribution in the development of safety actions and the areas we need to improve upon.
Each safety action and area for improvement identified will be listed within an Action Plan and include:
- A description.
- The person who will complete it - this is the action owner.
- A target date for it to be completed by.
- The date it was completed.
- How it will be measured.
- How often it will be measured or improvement monitored.
- Who will be responsible for monitoring the results.
- A planned review date.
Your investigation stage 5: writing the investigation report.
We use a national template to write the investigation report. The template is designed to make sure that all hospital Trusts are using a standard approach and that the report is of good quality.
The report will be written in clear, simple, everyday English (this can be translated at the patient/families’ request) whenever possible. We will avoid technical and medical language, but if we need to use this, we will provide an explanation.
We will ask you, how the person directly impacted by what happened (yourself or another), would like to be referred to in the report. We can use a preferred name or a generic term like ‘the patient’.
The report will include:
- An executive summary which is a short description of what happened, findings and areas for improvement.
- Background and context which is a short explanation of the subject under investigation.
- A description of the patient safety incident.
- The investigation approach which is an explanation how what happened was reported, how the decision was made to investigate, terms of reference, and how information was gathered.
- Findings which is an explanation of how the incident happened. It may include diagrams or tables to help explain the findings.
- A safety action summary table which is a list of areas for improvement which the investigation has identified, as well as specific actions.
- Appendices which will include any additional information to help understand the report.
Before the report is finalised, we will send you a draft version of the report.
It is important that we have explained your experience accurately and answered your questions as part of the terms of reference.
Once you have read the draft report, please talk to your Engagement Lead about the findings, especially if you disagree with them or if you have more questions.
You can write down anything you would like to talk about. Some prompts which may help you are provided below:
- Was there anything you did not expect to see in the report?
- Are there any points you disagree with in the report?
- Do you have any questions which the report does not answer?
The Patient Safety Incident Investigation (PSII) final report
Once feedback on the draft report has been written, it will be sent to the Trust’s Patient Safety, Governance and Legal teams who will read the report and provide feedback. This is to make sure that the report is of good quality and has identified the areas for improvement and actions.
You will then receive a copy of the final investigation report.
Your Engagement Lead will go through it with you. They can talk about what the investigation found and how actions for the Trust were decided.
Your Engagement Lead will ask you about any support you might need moving forward, and they will help you to organise this if you would like them to. Please see the section ‘your support needs’ further down.
You can write down the key details about the final investigation report if it would be helpful. We should have provided contact details of support available, and information about what to do if you are not happy about the conclusion of the investigation.
Your notes on the PSII final report can include:
- When you received a copy of the investigation report
- What the important parts of the final report are for you
Further involvement
Other investigations
In most cases, the end of this investigation process will mean that conclusions have been made about what happened.
However, there are cases in which further investigation are necessary. These might happen at the same time as the Trust investigation, or they might happen afterwards. For example, following an unexplained death, there will be an inquest led by the coroner, or following certain incidents in maternity services the Maternity and Neonatal Safety Investigations (MNSI) might carry out an independent Patient Safety Incident Investigation (PSII).
If your Engagement Lead knows there is going to be another investigation alongside or immediately after this one, they will tell you. They will also support you to find out more information about the additional investigation process if you would like to know more.
Opportunities for further involvement
Once the final investigation report is complete, this marks the end of the formal investigation process. For the Trust, this is the point at which we must start to implement the action plan included in the report.
It is important that we have support and guidance to do that. An organisation called the Integrated Care Board (ICB) monitor the actions from Patient Safety Incident Investigations (PSII). Trusts are expected to address these actions within specific timescales, based on how complex they are.
As a Trust, we have specific processes that we use to respond to actions. There may be instances where you are offered the opportunity to meet with our members of staff who are responsible for actions in the action plan. This might be more likely if you have specific information about ways the service could be changed or improved based on your experience of the Trust, and what happened. This will not always be possible, but you can speak to your Engagement Lead if this is something you would be interested in.
Your support needs
Being involved in a patient safety incident can be distressing and you may find the investigation process difficult. You can talk to your Engagement Lead about how you are feeling, and they may signpost you to:
Citizens Advice who can give high quality, independent advice about any problems or questions you might have. They can provide you with the knowledge and confidence to find a way forward. They have a network of national and local independent charities that can provide free and confidential advice. You can find out more at www.citizensadvice.org.uk. You can also call an advisor on 0800 144 8848.
Mind who is a registered charity who provide support and advice to anyone who is suffering with their mental health. If you have been affected emotionally following your experience or if you are finding the investigation process difficult, you can contact Mind. You can find general support resources and information about local services at www.mind.org.uk. You can also email them on info@mind.org.uk or call their helpline on 0300 123 3393.
Samaritans who are a registered charity providing support to anyone in emotional distress or anyone who is struggling to cope. If you have been emotionally affected by what happened, you can contact the Samaritans for free and there will always be someone there to listen to you and talk to you. You can find more information at www.samaritans.org. You can email them on jo@samaritans.org or you can call free on 116 123. Their support is available 24 hours a day, 7 days a week, 365 days of the year.
The Trust’s Bereavement team who are bereavement officers and specialist nurses. The team can support grieving families to make sense of what has happened and provide practical and emotional help. If your loved one has died, you will have been given a bereavement booklet that contains guidance and useful contacts. The Bereavement team can be contacted by telephone: 01524 512405, Monday - Friday 9 - 4pm.
The Trust Chaplaincy team who are trained and accredited hospital chaplains and volunteers that offer religious and pastoral support to patients and relatives. They are available to listen and support. The lead chaplain can be contacted by email: ian.dewar@mbht.nhs.uk or telephone: 01524 519231.
What if I’m not happy?
The investigation report should have answered most, if not all, of the questions you had about how and why the incident happened. However, in some cases you might still have questions that the Learning Response Lead was not able to include during the investigation, or questions that have arisen after reading the final report. Below are details of different organisations that you can access for support and guidance.
Action against Medical Accidents (AvMA) is a registered charity which aims to support people affected by avoidable healthcare harm. They can provide specialist, independent advice and support following patient safety events. Visit www.avma.org.uk.
Patient Advice and Liaison Service (PALS) is a free and confidential service run by the Trust and is part of the Patient Relations Department. You can talk to a PALS member and they will try to resolve your concerns as quickly as possible. PALS officers are available from 9am to 5pm, Monday to Friday. Telephone: 01539 715577 or email: PALS@mbht.nhs.uk.
Complaints
Everyone has a right to make a complaint about any aspect of NHS care, treatment or service. The NHS website gives guidance on how to do this and details of local advocacy providers at www.nhs.uk/using-the0nhs/about-the-nhs/how-to-complain-to-the-nhs.
A complaint can be raised by contacting the Trust’s Patient Relations team. There is a process in place to make sure complaints are dealt with in a confidential and sensitive way. To raise a complaint telephone: 01539 716621 or email:
commentsandcomplaints@mbht.nhs.uk.
If you do not feel able to raise a complaint directly with the Trust, you can also contact the Lancashire and Cumbria Integrated Care Board (ICB), further details can be found on their website: www.lancashireandsouthcumbria.icb.nhs.uk.
Local Healthwatch is an organisation that helps people speak up about health and social care in England. Healthwatch can give information about organisations that can help with the complaints process. There are two Healthwatch branches that cover our area:
- Healthwatch Lancashire telephone: 01524 239 100
- Healthwatch Westmorland and Furness telephone: 0300 373 2820
The Parliamentary and Health Service Ombudsman (PHSO) respond to unresolved complaints. They can support you if you have made a complaint and the organisation has not responded to your complaint, or if you are dissatisfied with their response. You can find more information at www.ombudsman.org.uk.
Key words and phases
- Action plan: The investigation may identify several immediate safety actions that need to be addressed. These actions will be listed with dates for completion and owner in a plan.
- Adverse event: An event which resulted in an undesirable clinical outcome which may have caused harm to a patient.
- Common themes: Common themes are recurring ideas, subjects or topics, relevant to what happened and the Terms of Reference. The investigator identifies themes when they are reading all the information they have collected about what happened.
- Coroner: A coroner is a government official or member of the judicial system who carries out inquests.
- Engagement Lead: The person who is responsible for engaging with and involving those affected by what happened.
- Governance team: Governance teams work in NHS organisations and are responsible for monitoring the quality of services and for safeguarding high standards of care.
- Health Services Safety Investigations Body (HSSIB): HSSIB is funded by the Department for Health and Social Care and is responsible for carrying out independent investigations into NHS-funded care across England.
- Integrated Care Board (ICB): The integrated care board is an NHS organisation responsible for developing a plan for meeting the health needs of the population.
- Inquest: An inquest is a formal investigation conducted to determine how someone died.
- Learning Response Lead: The person who is responsible for carrying out investigations for learning.
- Legal team: Most NHS Trusts have legal teams to manage a wide range of legal matters for the Trust including claims brought against the Trust; inquests; any proceedings involving Trust witnesses; medical treatment applications to the High Court; and medical records requests from solicitors.
- Maternity and Neonatal Safety Investigations (MNSI): Independent investigations into certain patient safety events that happen in maternity care. Where relevant MNSI will make safety recommendations to improve services at local level and across the whole maternity healthcare system in England.
- Near miss: An event that does not cause harm, but which has the potential to cause injury or ill health if it had not been caught in time.
- Never event: Serious, largely preventable patient safety events that should not occur if the available preventative measures have been implemented.
- Patient safety event: A reportable event that is a risk to patient safety, including patient safety incidents, which are unintended or unexpected events in healthcare that could or did harm one or more patients.
- Patient Safety Specialist: Individuals in healthcare organisations who have been designated to provide senior patient safety leadership.
- Patient Safety Partners: Patients, carers and other members of the public that support and contribute to a healthcare organisation’s governance and management processes for patient safety.
- Patient Safety team: Most NHS Trusts will have a patient safety team dedicated to working within the service to minimise the risk and impact of patient safety events.
- Policy: An official document that includes a set of guidelines to guide decisions and achieve specific outcomes.
- Quality Improvement Project (QIP): The investigation may identify areas for improvement; these will be managed as a project to achieve an aim that intends to improve the identified area of concern.
- Report: A written account of your investigation.
- Risk analysis: Risk analysis involves finding things and situations that could potentially cause harm to people.
- Terms of Reference: These are guidelines that define the scope and purpose of the investigation.
How you can give feedback
Thank you for being part of the investigation.
We welcome your time in providing feedback on your Patient Safety Incident Investigation (PSII) and how we have engaged with you.
You can share your feedback by visiting www.forms.office.com/e/4tDkk1KUuY.
If you require any support to share your feedback or to receive a paper copy, please contact a member of the Patient Experience team on 01229 404434.
Your input is invaluable in helping us improve our processes and approach for the future to ensure we meet the needs of all families and patients within the Patient Safety Incident Response Framework (PSIRF). The information you provide will be used internally for improvement purposes only.
There are five questions in the feedback form:
1. Your name.
2. To what extent do you agree/disagree with the following statements:
- The apology received was meaningful and appropriate.
- The approach taken was individualised and considered my individual circumstances and needs.
- The timescales for the investigation were discussed with me and I was kept informed of progress.
- During the investigation, I was treated with respect, kindness, and compassion.
- Guidance and clarity were provided throughout the investigation process.
- During the investigation process, my voice was heard.
- The investigation process felt collaborative and open.
- The PSII Guide was a useful and supportive document to refer to.
3. Please share your views on the aspects of the investigation engagement process you felt went well.
4. Please share your views on the areas where you feel we could have done better.
5. Please share any other feedback you would like us to consider.

